Multidrug-Resistant Bacteria

What Are Multidrug-Resistant Bacteria?
Multidrug-resistant (MDR) bacteria are those that have developed resistance to three or more different groups of antibiotics, making them difficult or even impossible to treat with the medications commonly used to combat bacterial infections. If bacteria are resistant to all available antibiotics without exception, they are referred to as pandrug-resistant (PDR) bacteria.
Multidrug-resistant bacteria often emerge due to the inappropriate or excessive use of antibiotics, whether in humans, animals, or the environment. Examples include Escherichia coli and Pseudomonas aeruginosa resistant to carbapenems, or methicillin-resistant Staphylococcus aureus (MRSA).
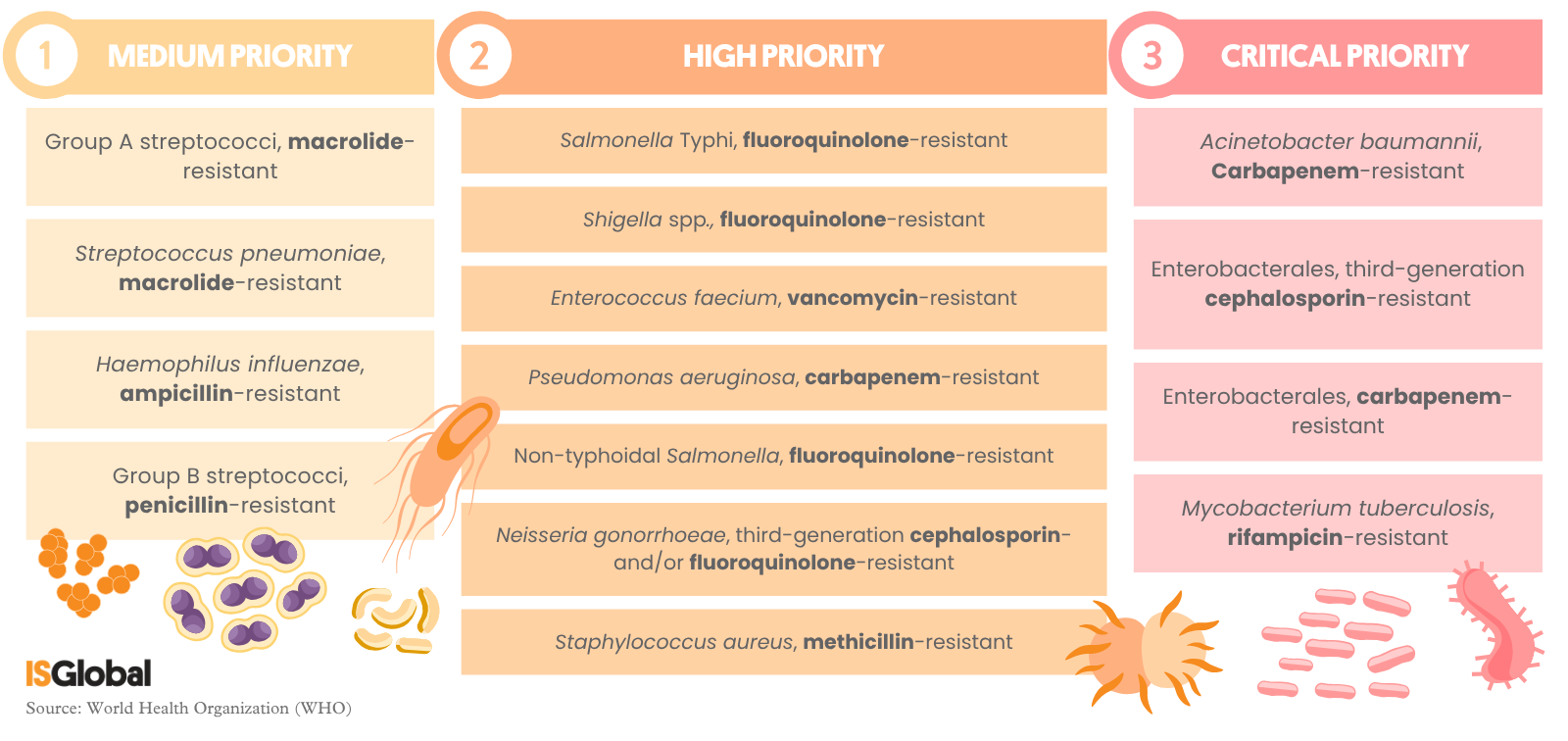
The World Health Organization (WHO) has classified drug-resistant bacteria into three priority levels based on their impact on public health:
- Medium priority: Includes bacteria that cause diseases with a significant burden of morbidity and mortality, particularly in vulnerable populations such as children and the elderly. Although not currently posing as critical a threat as those in higher categories, they require ongoing epidemiological surveillance to prevent an increase in antibiotic resistance.
- High priority: Comprises pathogens responsible for severe infections in hospitals and the community, generating a high burden of disease and death, especially in low- and middle-income countries. Some of these bacteria have developed resistance to multiple antibiotics, complicating treatment and demanding urgent public health action.
- Critical priority: Includes bacteria that pose the greatest threat to public health due to their resistance to last-resort antibiotics, their high transmissibility, and the difficulty of treating them with current therapeutic options. Some may be pandrug-resistant.
A Threat to Public Health
Multidrug-resistant bacteria represent a serious threat to public health, as they limit available treatment options and increase the risk of spreading difficult-to-treat infections. This can lead to prolonged illness, increased mortality, and complications during routine medical procedures such as surgery or cancer treatment. As a result, diseases that we currently treat easily with antibiotics could become extremely hard to manage.
The rise in antibiotic resistance also results in high economic costs: more expensive drugs are used, hospital stays become longer, and stricter control measures are needed.
Tackling this issue is essential to safeguard the effectiveness of antibiotics in the future, protect vulnerable populations, and preserve modern medicine’s ability to treat infectious diseases effectively. Therefore, raising awareness, using antibiotics responsibly, preventing infections, and adopting global policies are all crucial.
READ MORE
COLLAPSE
- New Antibiotics Against Bacterial Resistance: the Potential of Gold Molecules(ISGlobal, 2025)
- Antimicrobial Resistance: The Silent Pandemic?(ISGlobal, 2024)
- Antibiotics: What Happens If You Take Them Late or Expired? 7 Questions Answered(ISGlobal, 2023)
- Promising Treatments Against Resistant Bacteria: Research on New Antibiotics and Alternatives for Microbial Infections(ISGlobal, 2022)
- A Promising New Synthetic Peptide to Combat Multidrug-Resistant Bacteria(ISGlobal, 2022)
MULTIMEDIA MATERIAL