Antibiotic resistance
What is antibiotic resistance?
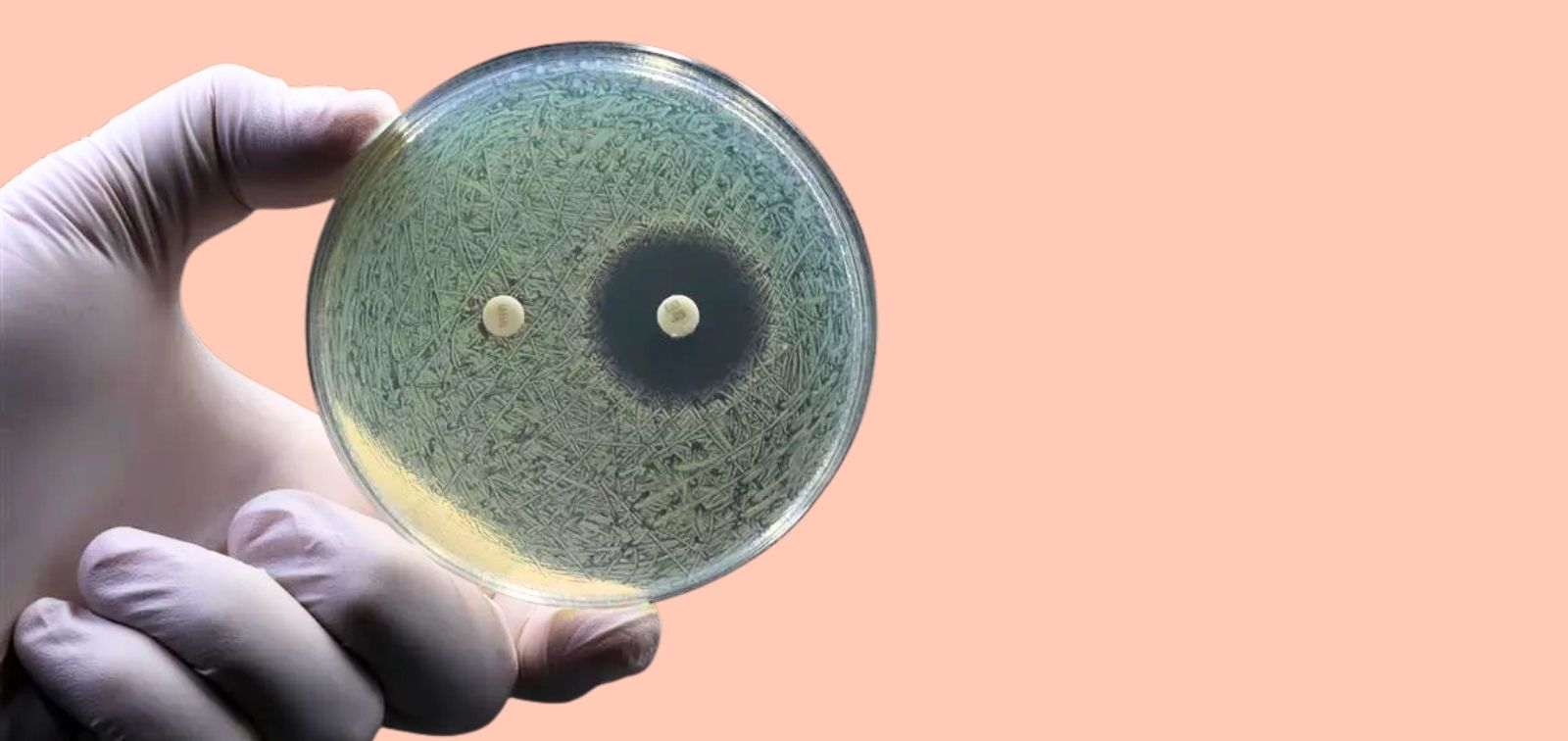
Antibiotic resistance is the ability of some bacteria to survive and continue multiplying despite the presence of antibiotics that were previously effective in killing them. This happens through genetic mutations or by acquiring resistance genes.
Drug-resistant bacteria can cause infections in humans, animals, and plants that are far more difficult to treat than non-resistant infections.
- If these bacteria are resistant to three or more antibiotic classes, they are known as multidrug-resistant bacteria (MDR).
- If they are resistant to all but one or two antibiotic classes, they are called extensively drug-resistant bacteria (XDR).
- If they are resistant to all available antibiotic families without exception, they are known as pandrug-resistant bacteria (PDR).
The silent pandemic
Antibiotic resistance is currently one of the greatest threats to global health. It limits treatment options and increases morbidity and mortality rates from resistant infections. Infections such as sepsis, and diseases like tuberculosis, pneumonia or gonorrhoea, are becoming harder to treat. For this reason, antibiotic resistance is also known as the silent pandemic, and it has the potential to become the leading global cause of death by 2050.
It can affect anyone, regardless of age or location. In places where antibiotics are available without prescription (for humans, animals, or crops), the issue worsens. In countries without standardised clinical guidelines, overprescription by healthcare and veterinary professionals is common. Even within the EU, variations in prescription regulation make overuse harder to control.
Although antimicrobial resistance is a natural process, the misuse of antibiotics is accelerating it, putting not only human health but also ecosystems and planetary health at risk. That’s why responsible use of antibiotics is essential to preserve their effectiveness and protect global health.
Guidelines from the World Health Organization (WHO)
- Only take antibiotics when prescribed by a qualified healthcare professional.
- Do not request antibiotics if your healthcare provider says they’re unnecessary.
- Always follow your doctor’s instructions regarding antibiotic treatments.
- Do not use leftover antibiotics from previous treatments. Return them to a pharmacy disposal point.
- Prevent infections through frequent handwashing, avoiding contact with sick people, practising safe sex, not sharing personal items (like glasses or razors), and keeping up with recommended vaccinations.
- Prepare food hygienically: keep hands and surfaces clean, separate raw and cooked food, cook meat thoroughly, keep food at safe temperatures, and use clean water and safe ingredients.
- Stay informed: in case of doubt, contact a healthcare provider.
In addition to the general population, healthcare professionals, agricultural workers, and policy-makers play a crucial role in reducing the impact and spread of antimicrobial resistance. There is an urgent need to transform how antibiotics are prescribed and used. Even with new drugs in development, antibiotic resistance will remain a serious threat unless practices are changed.
READ MORE
COLLAPSE
- Antimicrobial Resistance: The Silent Pandemic?(ISGlobal, 2024)
- Many of the Barriers to Combating Antimicrobial Resistance Are Common to All European Countries(ISGlobal, 2023)
- AMR EDUCare, A New EU-Wide Project to Train Over 4,000 Health Professionals on Antimicrobial Resistance(ISGlobal, 2023)
- Antimicrobial Resistance: A Threat that Calls for Non-Conventional Strategies(ISGlobal, 2019)
MULTIMEDIA MATERIAL
