Chikungunya
What Is Chikungunya?
Chikungunya fever is an illness caused by the chikungunya virus. It is transmitted through the bite of infected mosquitoes, and was first described in 1952 in the United Republic of Tanzania. “Chikungunya” comes from the kimakonde language (spoken in parts of Tanzania and Mozambique) and means “to become contorted“, referring to the posture of those affected, who often hunch over due to intense joint pain.
The chikungunya virus is an RNA virus, meaning it stores its genetic information in a ribonucleic acid (RNA) molecule rather than in DNA (deoxyribonucleic acid). Other RNA viruses, such as Dengue and Zika, can cause symptoms similar to chikungunya, sometimes making diagnosis more difficult.
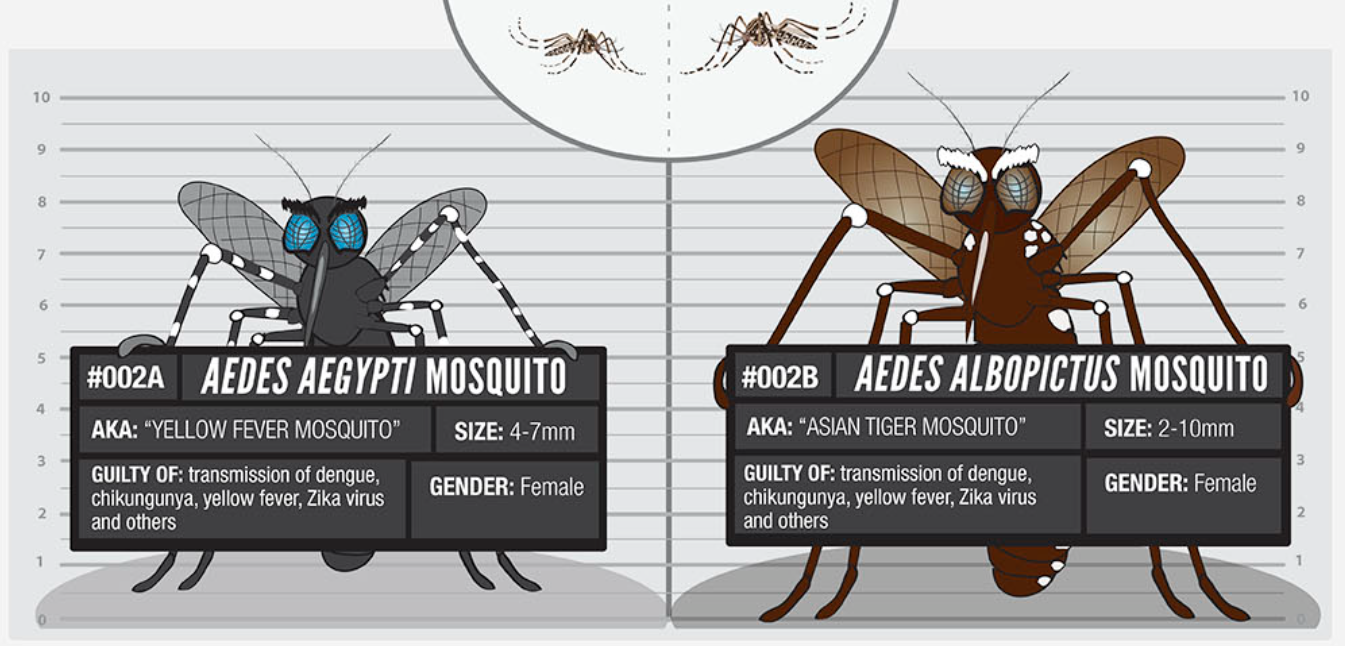
Transmission
Chikungunya virus is transmitted by mosquitoes, primarily by the species Aedes aegypti and Aedes albopictus. These mosquitoes, which typically bite during the day, lay eggs in stagnant water.
A mosquito can become infected by biting an infected person. Once inside the mosquito, the virus replicates (makes many copies of itself), and when the mosquito bites another person, it transmits the infection. This perpetuates the transmission cycle.
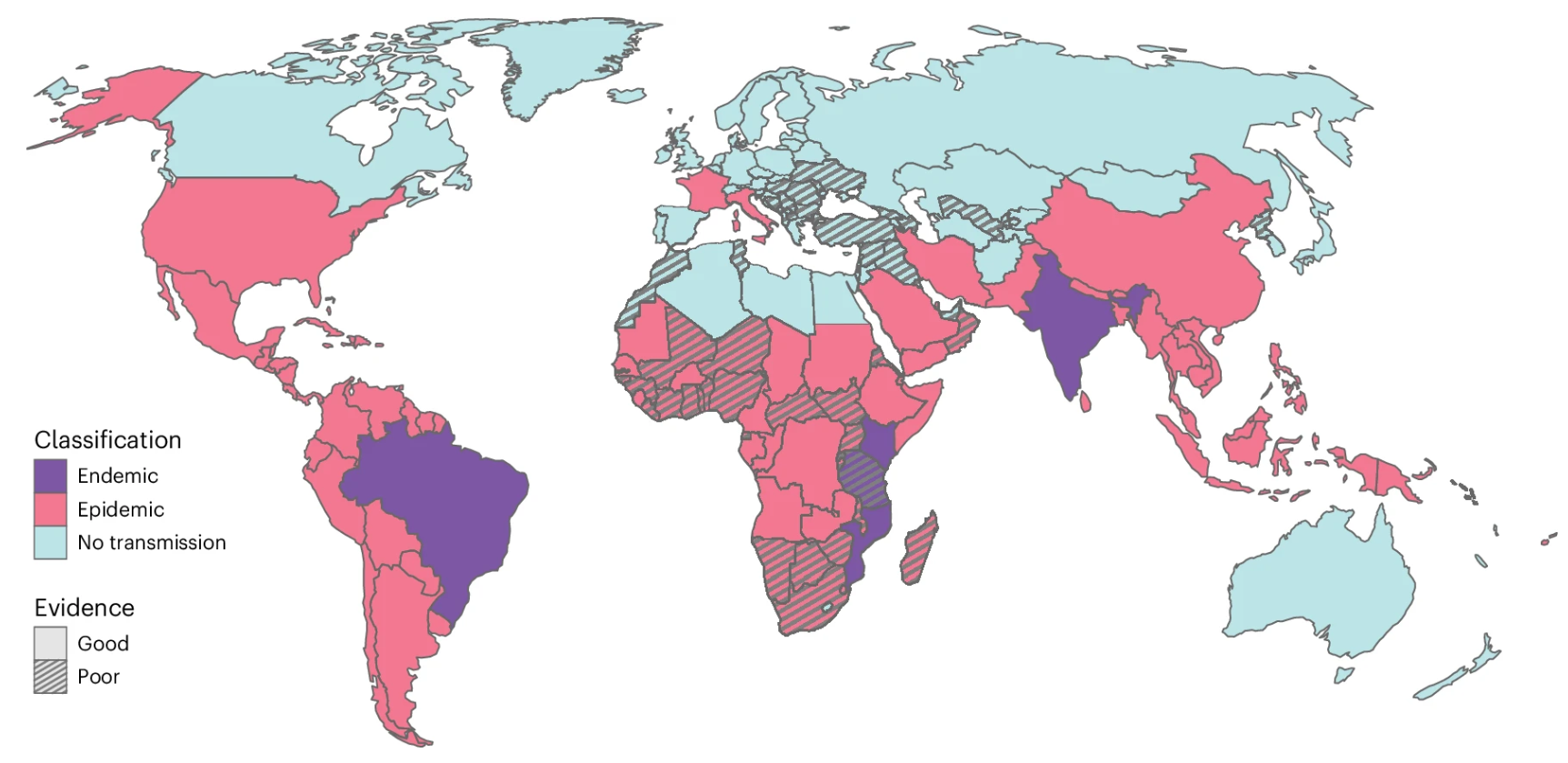
Epidemiological situation of chikungunya in 2025
In recent years, and especially during 2025, chikungunya has experienced a resurgence in various parts of the world. Although it was historically confined to Africa, where it still circulates in natural cycles between primates and mosquitoes, today autochthonous transmission has been recorded in 119 countries and recent outbreaks have occurred in regions such as the Indian Ocean islands, China, Madagascar, Somalia, Kenya, India and several European countries.
The Americas currently account for the highest number of reported cases, reflecting the widespread circulation of the virus in a continent where, together with Africa and Southeast Asia, the majority of the estimated 35 million annual infections occur. Between January and September 2025, more than 445,000 suspected and confirmed cases and 155 deaths were reported, although the true burden may be higher due to limited surveillance in several regions, including Africa. The spread of Aedes mosquitoes, favoured by climate change, rapid urbanisation and increased travel, is enabling the virus to reach areas previously unaffected.
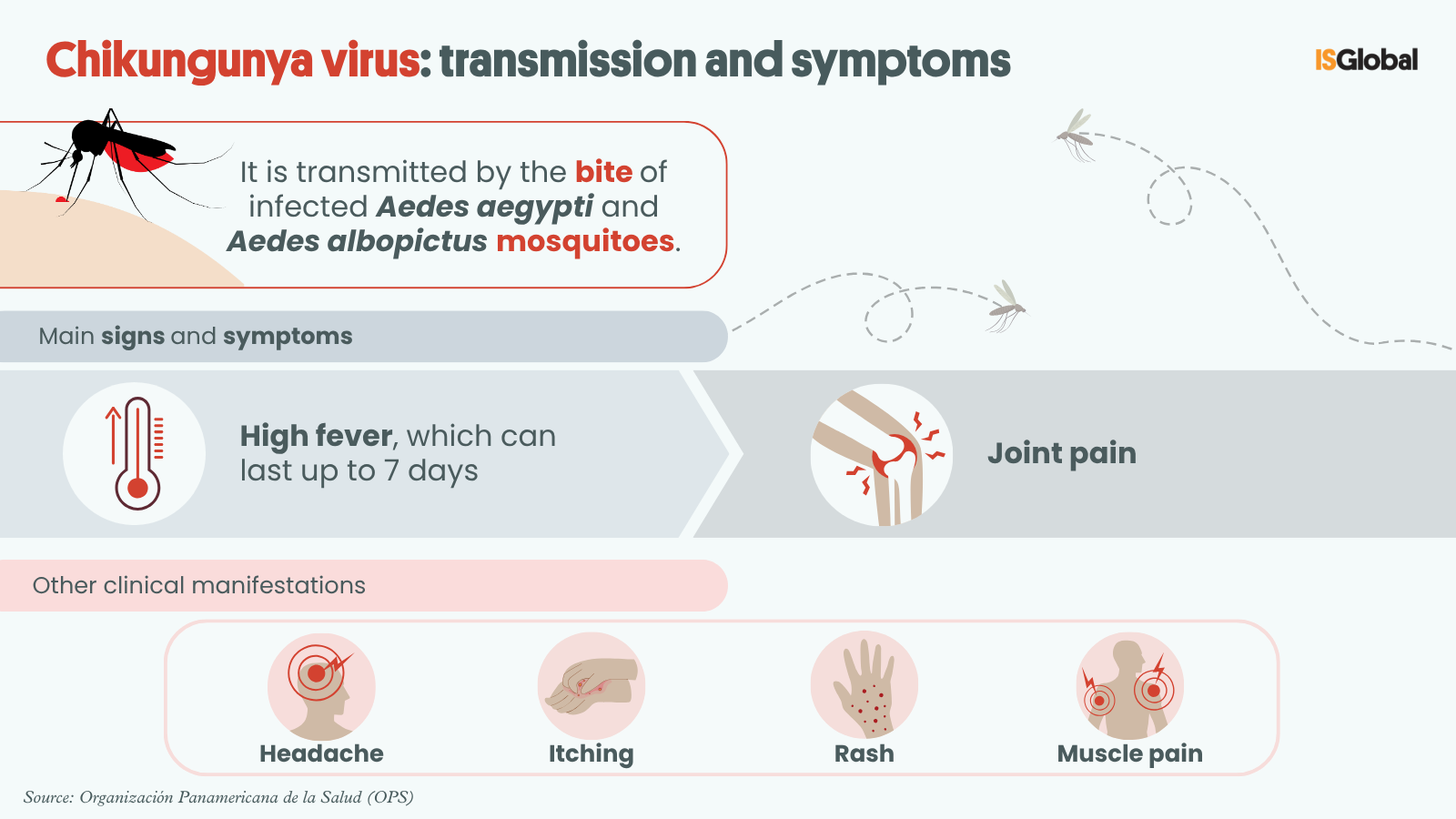
Symptoms
In symptomatic patients, chikungunya fever usually appears four to eight days after the bite of an infected mosquito. The illness is characterised by the sudden onset of fever, often accompanied by severe joint pain, which can be disabling. While the joint pain usually resolves in a few days, in some cases it can persist for weeks, months, or even years. Other common symptoms include muscle pain and headaches.
Most patients recover fully. However, complications have occasionally been reported affecting the eyes, heart, or nervous system. Newborns infected during childbirth and older adults with pre-existing conditions are at greater risk of developing severe forms of chikungunya. In these cases, complications can be more serious and increase the risk of death.
Diagnosis
To detect chikungunya virus, a blood sample can be analysed during the first week of illness. One of the most widely used tests is RT-PCR, a molecular technique that detects the virus’s genetic material and confirms infection with precision.
In later stages of the disease, chikungunya can be diagnosed by detecting the presence of antibodies against the virus in the blood.
Treatment
There is currently no approved antiviral treatment specifically for chikungunya. Management focuses on relieving symptoms such as fever and joint pain using painkillers, antipyretics, rest, and hydration.
Prevention
The best way to prevent chikungunya fever is to avoid mosquito bites. It’s also vital to protect infected patients from mosquito exposure during the first week of illness to break the transmission cycle. It is recommended to wear long-sleeved clothing, use approved repellents, and install screens on doors and windows to keep insects out.
To reduce mosquito populations, it is important to empty and clean containers that hold water weekly, dispose of items that collect water, and support local vector control campaigns. In outbreak situations, insecticides may be used.
Currently, two vaccines for chikungunya have been developed.
In 2023, the United States Food and Drug Administration (FDA) approved Ixchiq, the first vaccine for individuals aged 18 and over. The European Commission authorised its marketing in 2024. It contains a live attenuated virus and is administered as a single dose. Although it has shown high efficacy, its use has been restricted in older adults (60–65 and above) due to reports of serious adverse events, especially in individuals with underlying conditions.
In January 2025, the European Medicines Agency (EMA) recommended authorisation of a second vaccine, Vimkunya, intended for adolescents aged 12 and up, as well as adults. This vaccine uses virus-like particles (VLPs) that mimic the virus’s structure, making it safer, especially for immunocompromised individuals. It is also administered as a single dose. Vimkunya was approved in the United States in February 2025 and is awaiting final approval by the European Commission for marketing in the European Union.
Vaccination is recommended before travelling to areas where chikungunya is endemic or where outbreaks are occurring. Although these two chikungunya vaccines have gained regulatory approval in some countries, they remain unavailable for widespread use and are yet to be broadly accessible in affected regions.
READ MORE
COLLAPSE