Malaria
What Is Malaria?
Malaria, also known as paludism, is a potentially deadly parasitic disease caused by protozoa of the Plasmodium genus. In humans, the disease can be caused by five different species: Plasmodium falciparum, Plasmodium vivax, P. malariae, P. ovale, and P. knowlesi. Of these, P. falciparum is the most deadly, while P. vivax is the most widely distributed worldwide. Transmission mainly occurs through the bite of infected Anopheles mosquitoes.
Children under five, pregnant women, infants, as well as travellers and people living with HIV, are at greater risk of developing severe infection.
According to the 2024 World Malaria Report, there were 263 million cases in 2023, causing 597,000 deaths. Africa accounted for approximately 94% of cases and 95% of deaths—around 76% of them in children under five. The countries with the highest malaria mortality were Nigeria, the Democratic Republic of the Congo, Niger, and the United Republic of Tanzania.
Transmission
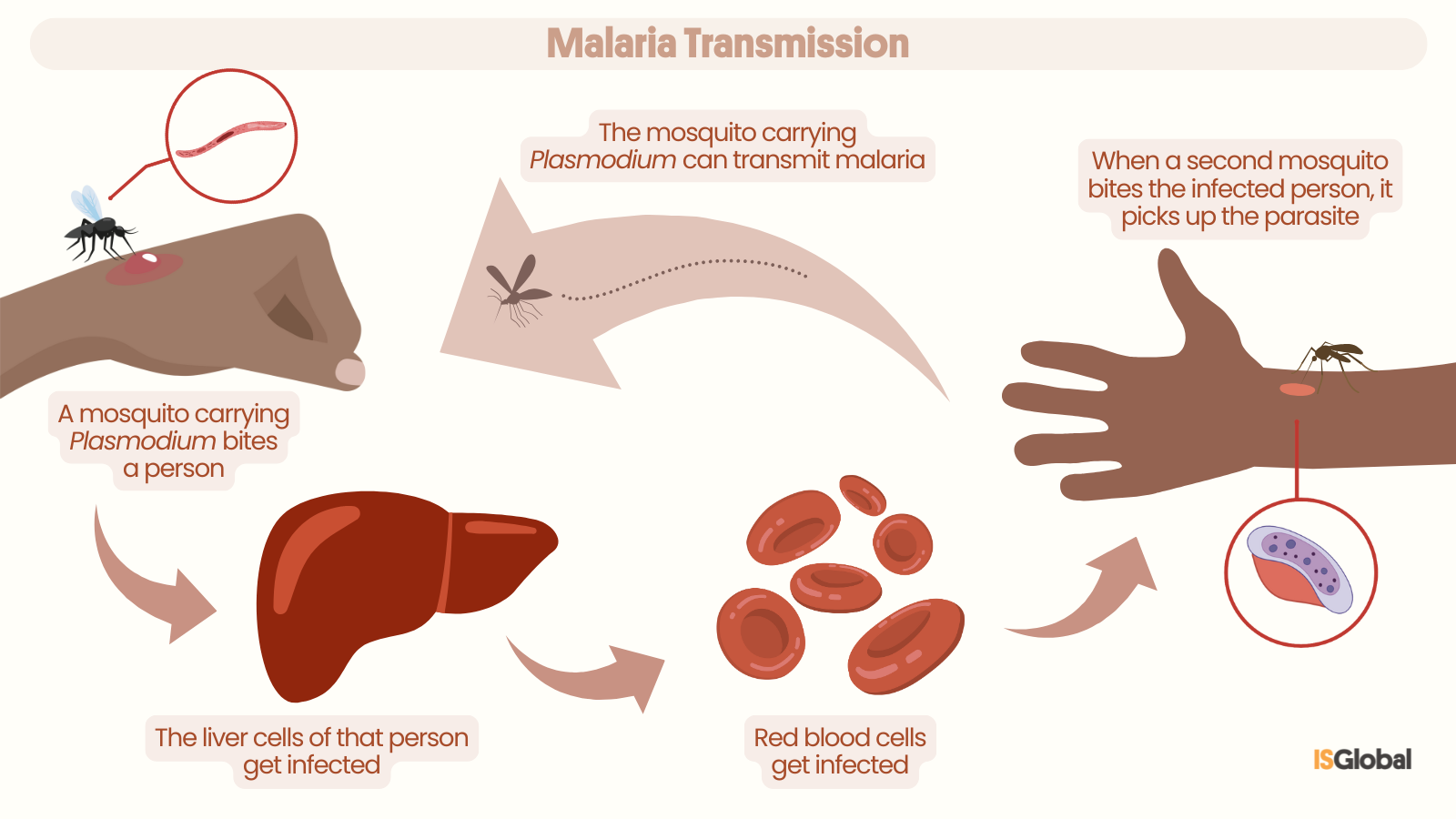
In most cases, malaria is transmitted by the bite of a female Anopheles mosquito, which acts as a vector by transmitting the Plasmodium parasite to humans. These mosquitoes acquire the parasite when they bite an infected person. When they then bite a healthy person, the parasites are transmitted into the bloodstream, infecting liver cells and later red blood cells.
Mosquitoes are most often found in rural areas and bite mainly between dusk and dawn. Climatic conditions such as temperature and humidity affect their survival and activity. Less common routes of transmission include blood transfusions, organ transplants, and contaminated needles. During pregnancy or childbirth, an infected woman can also pass the parasite to her baby—this is known as vertical or congenital transmission.
Symptoms
Symptoms usually appear 10–15 days after the mosquito bite but may emerge over a month later.
Early symptoms include fever, headache, and chills. Prompt treatment can prevent the infection from becoming severe. If not diagnosed and treated within the first 24 hours, malaria can progress to severe symptoms such as extreme fatigue, seizures, bleeding, or difficulty breathing—and may even be fatal.
Malaria infection during pregnancy can also lead to premature birth or low birth weight in newborns.
However, it is important to note that not all infected individuals develop symptoms, which makes elimination of the disease more challenging.
Diagnosis
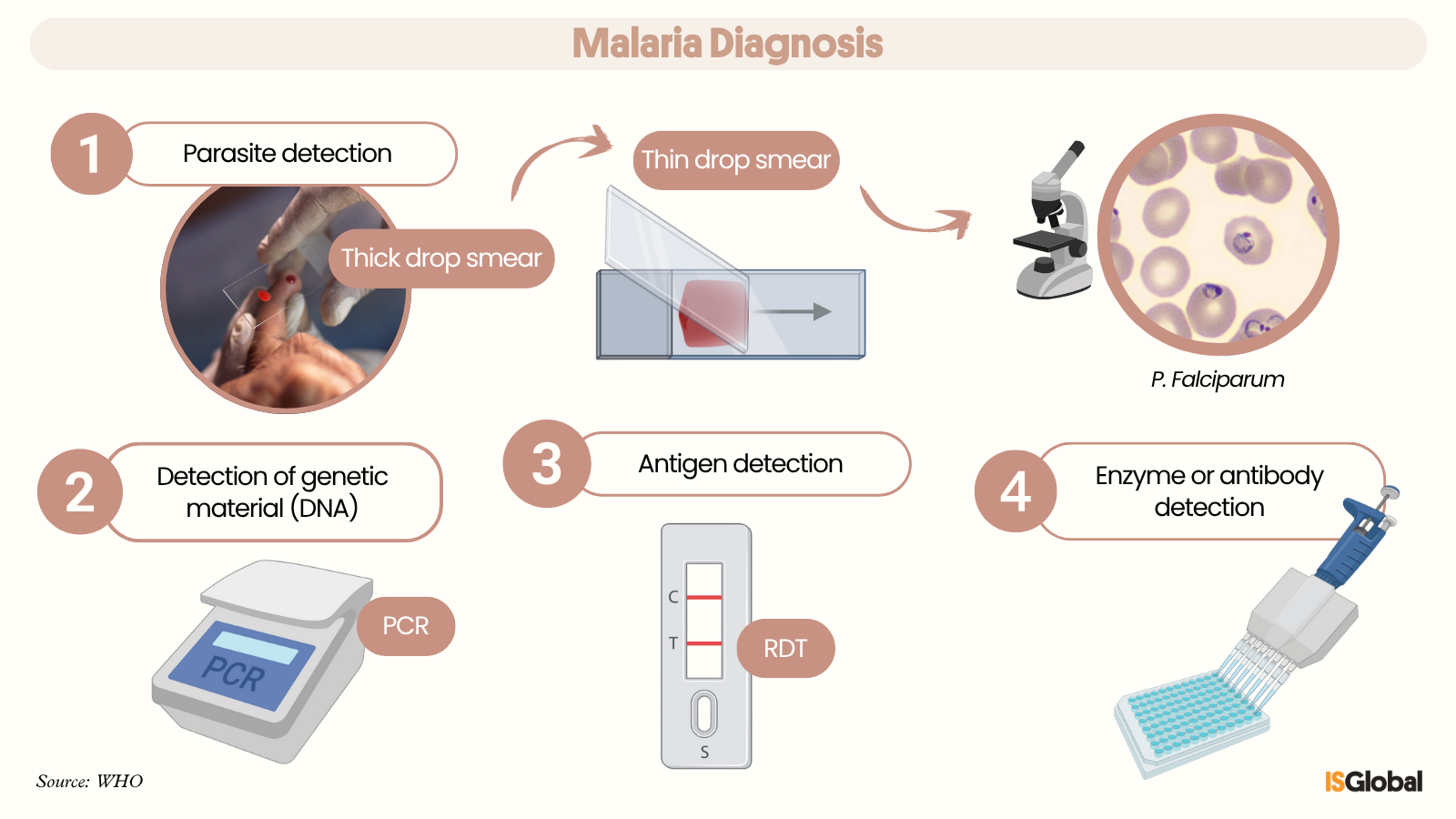
The gold-standard test for malaria diagnosis is the thick blood smear, where a drop of blood (usually from a fingertip) is placed on a slide, examined under a microscope, and checked for the presence of parasites. A thin blood smear may also be performed to identify the Plasmodium species in red blood cells and to estimate parasite load.
Molecular techniques (PCR) can also be used to detect the parasite’s genetic material (DNA) in a blood sample.
Rapid diagnostic tests (RDTs) detect parasite antigens in the patient’s blood.
Other indirect methods include analysing parasite enzymes or detecting antibodies against the parasite.
Treatment
Medicines used to treat malaria vary depending on factors such as disease severity and the Plasmodium species involved.
- Artemisinin-based therapies are effective against P. falciparum. However, resistance to artemisinin has begun to emerge in Southeast Asia, posing a global threat.
- Chloroquine was historically the main treatment until resistance developed in many regions. It is now recommended for treating P. vivax infections—except in areas with documented resistance, such as Indonesia.
- Primaquine or tafenoquine is used alongside chloroquine to prevent relapses, particularly in patients infected with Plasmodium vivax.
Treatment may be administered orally or intravenously. In cases of severe malaria, supportive care and monitoring in an intensive care unit may be required.
Prevention
To prevent malaria, it is crucial to avoid mosquito bites—this is known as vector control. Recommended measures include:
- Installing window screens.
- Using insecticide-treated bed nets.
- Applying tropical-strength mosquito repellents.
- Using indoor sprays and fumigation.
- Wearing lightweight, long-sleeved clothing.
Travellers to malaria-endemic areas should consult healthcare providers about starting preventive (prophylactic) treatment.
Are there any vaccines for malaria?
Since October 2021, the WHO has recommended widespread use of the RTS,S/AS01 vaccine in children living in areas with high transmission of Plasmodium falciparum. This vaccine has been shown to reduce both cases and severe forms of the disease. In 2023, a second vaccine—R21/Matrix-M—was approved, which is also safe and effective. Both are now being integrated into child vaccination programmes across Africa and have the potential to save tens of thousands of lives annually.
READ MORE
COLLAPSE
- A New Weak Spot Found in the Malaria Parasite(ISGlobal, 2025)
- New Study Sheds Light on How the Malaria Parasite Controls Its Genes(ISGlobal, 2025)
- Malaria: The Canary in the Global Health Mine(ISGlobal, 2025)
- 'Plasmodium vivax', a Human Malaria Parasite Resilient to Elimination(ISGlobal, 2024)
- Maternal Antibodies Interfere with Malaria Vaccine Responses(ISGlobal, 2024)
- Malaria Elimination(ISGlobal)
- Path to Zero: Guiding malaria elimination efforts in Mozambique and beyond(ISGlobal)
MULTIMEDIA MATERIAL

